Original scientific article
Local infusion of Staphylococcus aureus into the porcine internal carotid artery as a model of sepsis-related brain abscesses – a pilot study
by Lærke B. Astrup1,2*, Tine M. Iburg1,2, Jørgen S. Agerholm1,3, Bent Aalbæk1, Henrik E. Jensen1, Ole L. Nielsen1, Pall S. Leifsson1
1Department of Veterinary and Animal Sciences, Faculty of Health and
Medical Sciences, University of Copenhagen, Grønnegårdsvej 15,
DK-1870 Frederiksberg C, Denmark
2Section for Diagnostics and Scientific Advice, National Veterinary
Institute, Technical University of Denmark, Anker Engelunds Vej,
2800 Lyngby, Denmark.
3Department of Veterinary Clinical Sciences, Faculty of Health and
Medical Sciences, University of Copenhagen, Dyrlægevej 68, DK-1870
Frederiksberg C, Denmark.
 Correspondence: Lærke B. Astrup (boyeastrup@gmail.com)
Correspondence: Lærke B. Astrup (boyeastrup@gmail.com)
Department of Veterinary and Animal Sciences,
Faculty of Health and Medical Sciences,
University of Copenhagen,
Grønnegårdsvej 15, DK-1870 Frederiksberg C,
Denmark
Summary
Brain pathology is an important aspect of human sepsis but is difficult to study in human patients. Therefore, animal models of sepsis-related brain pathology are needed. As pigs mirror multiple aspects of sepsis-related brain pathology in humans, this makes the pig a potentially suitable model. Unfortunately, models of sepsis in pigs are difficult to manage due to the accompanying massive systemic inflammatory response. To overcome these difficulties we designed a model in pigs of brain bacteremia established by local brain infusion in order to evaluate if this approach could reduce the systemic responses but still reflect the brain pathology of sepsis in humans. As a pilot study to obtain basic knowledge, we evaluated two methods of local infusion: long term infusion (60 minutes) of Staphylococcus aureus suspended in saline and, short-term infusion (10 minutes) of S. aureus embedded in autologous microthrombi.
The study revealed: 1) bacteria suspended in saline as well as embedded in microthrombi can pass through the rete mirabile and thereby cause local brain bacteremia; 2) despite the high dose of S. aureus used for infusion, only mild clinical signs developed; and 3) despite the mild clinical signs, one pig had developed a brain microabscess by 48 h after infusion. The brain pathology present in this pig thereby reflected human cases of S. aureus-sepsis with microabscess formation as the predominant lesion. In addition, the abscess morphology mirrored previously observed microabscesses in experimental porcine S. aureus sepsis models.
Introduction
During sepsis, brain microabscesses may develop as bacteria are transported hematogenously to the brain, either as free bacteria or within emboli. The development of brain microabscesses characterizes sepsis-related brain lesions in man (Pendlebury et al., 1989; Sharshar et al., 2004). However, the development of sepsis-related brain pathology is difficult to study in detail in human patients thus necessitating animal models (Pendlebury et al., 1989; Sharshar et al., 2003). The pig is a suitable model animal as brain microabscesses have been shown to develop in various scenarios of blood-borne spread of bacteria to the porcine brain (Bogdanski et al., 2000; Astrup et al., 2013; Christiansen et al., 2013a), similar to that described in humans. Furthermore, the well-established association between infective valvular endocarditis and the development of brain microabscesses in humans has been observed in experimental porcine sepsis as well (Tunkel & Kaye, 1993; Azuma et al., 2009; Christiansen et al., 2013a). Unfortunately, models of sepsis in pigs are difficult to manage due to the development of a massive systemic inflammatory response, which causes both animal welfare concerns and technical challenges (Nemzek et al. 2008; Leifsson et al., 2010; Soerensen et al., 2012). We hypothesized that these difficulties might be reduced by a local model approach. A local model approach that applies infusion of bacteria directly into the blood supply of the brain will provide two advantages. 1) Local infusion will ensure a full-dose exposure of bacteria to the brain. 2) Local infusion will concurrently reduce the systemic exposure as the infected blood is filtered through the lungs before entering the systemic circulation, thus presenting the blood to the pulmonary intravascular macrophages, which rapidly eliminate large quantities of bacteria from the blood (Soerensen et al., 2012). However, it is difficult to establish local infusion of bacteria to the porcine brain as pigs have a microarteriolar meshwork - the rete mirabile - at the vascular entrance to the brain (Haaland & Orderud, 1995). The rete mirabile hinders insertion of intra-arterial microcatheters beyond the level of the internal carotid artery (ICA) in pigs (Reinert et al., 2005).
We therefore conducted a pilot study based on three pigs to
investigate if it is possible to establish local brain bacteremia
through infusion of S. aureus into the ICA without causing
severe sepsis.
Methods
Animal ethics
The study was approved by the Danish Animal Experimental Inspectorate,
Danish Ministry of Food, Agriculture and Fisheries (license no.
2010/561−1916). The following humane end-points were applied:
reluctance to eat, drink, rise and move normally. These humane
endpoints were assessed as described below in the
“post-operative procedures” section.
Overall experimental design
During anesthesia, pigs were infused with S. aureus directly
into the ICA. Two infusion methods were tested: long-term infusion (60
minutes) of bacteria suspended in saline (Pig 1) and short-term
infusion (10 minutes) of bacteria embedded in autologous microthrombi
(Pigs 2 and 3). The pigs were allowed to recover from anesthesia and
were monitored until euthanasia after 24 h (Pigs 1 and 2) or 48 h (Pig
3). Then pigs were necropsied and examined by histology,
immunohistochemistry (IHC) and bacteriological culture.
Animals
Three male Göttingen minipigs (Ellegaard Göttingen Minipigs A/S,
Dalmose, Denmark) at the age of 2 months and with a bodyweight (BW) of
4.5-5.5 kg were used. The pigs were housed in the Laboratory Animal
Isolation Unit at the University of Copenhagen during the entire
study. The stables had a 12/12 h light rhythm and the area per pig was
3.41 m2. The pens were provided with abundant straw bedding and pig
toys. The pigs were acclimatized for 7 days and fed the same diet as
used by the pig supplier. The pigs were clinically examined 48 h
before infusion and a blood sample was taken. They were fasted for 24
h before surgery, but had access to water ad libitum at all
times. The pigs were housed together until surgery. After surgery and
throughout the study period the pigs were housed in single animal
units.
Inoculum
Staphylococcus aureus strain S54F9, spa type t1333
(Nielsen et al., 2009; Hasman et al., 2010) was used.
For long-term infusion, a suspension of 107 colony forming units (CFU)
S. aureus/ml was prepared. Each pig was inoculated with 10
ml/kg BW.
For short-term infusion,9 ml autologous blood was mixed with 1 ml
bovine thrombin (200 IU/ml) and 0.1 ml suspension of
S. aureus (108 CFU/ml). In this way, the total concentration
of infused bacteria was 108 CFU/kg BW in both infusion methods.
The blood used for microthrombi formation was drawn from the external
jugular vein (EJV) catheter into a syringe. The syringe was
immediately disconnected from the catheter and connected to a 150 mm
polyethylene catheter (PP10; inner diameter 0.28 mm, Polysan, Værløse,
Denmark). A syringe containing the thrombin and bacteria was inserted
at the other end of the catheter. Blood and the thrombin-bacteria
mixture were then circulated between the two syringes through the
catheter several times to assure thorough mixing. Then the mixture was
allowed to coagulate for 30 min. The coagulum was transected into
microthrombi by transferal through a sieve (mesh width 0.5 x 0.5 mm)
into a Petri dish. Saline was added to the microthrombi until a total
volume of 1.67 ml/kg BW was achieved. The microthrombi suspension was
aspirated into a sterile syringe and connected to the catheter in the
ICA and used for infusion.
Experimental procedures
The pigs were sedated by a mixture of 125 mg tiletamine hydrochloride (Zoletil 50 Vet, Virbac, Carros, France), 125 mg zolazepam hydrochloride (Zoletil Vet, Virbac), 125 mg xylazine hydrochloride (Rompun Vet, Bayer, Denmark), 125 mg ketamine (Ketaminol Vet., MSD Animal Health, Copenhagen, Denmark), 20 mg butorphanol tartrate (Morphasol Vet, BioVet, Fredensborg, Denmark) and 20 mg methadone hydrochloride (Comfortan Vet., Dechra Veterinary Products, Shrewsbury, UK). The sedation mixture was given at a dose of 1 ml/10 kg BW intramuscularly (IM). After sedation, pigs were anesthetized with propofol 1 mg/kg BW (Rapinovet ®; Schering-Plough , Farum, Denmark) through an ear vein catheter. Then pigs were intubated. Respiration- and heart rates and blood pressure were monitored automatically (Datex-Ohmeda Monitor, GE Healthcare, Brøndby, Denmark). The core temperature was maintained at 37 ± 0.5 °C during anesthesia (3M Bair Hugger, 3M Health Care, UK). When aseptically prepared for surgery, the ventral midline, the right lateral and the right dorsal surfaces of the neck were each injected with 1 ml lidocaine subcutaneously (SC) (Lidocain 10 mg/ml, SAD, Amgros I/S, Copenhagen, Denmark). A 5 cm midline incision was made in the ventral neck. Through blunt dissection, the vagal nerve, the common carotid artery and the EJV were displayed on the right side of the neck. The EJV was ligated and a catheter (0.8 PVC phthalate-free tube with X-ray line; Unomedical Inc., McAllen, USA) was guided to the cranial thoracic aperture and fixed by ligation to the vein and flushed with heparinized saline (2500 IU/ml). The free end of the catheter was tunneled SC to the right dorsal side of the neck where it was displayed via a 1 cm incision and fixed to the skin. The common carotid artery was ligated and a catheter (0.5 PVC phthalate-free tube with X-ray line; Unomedical Inc., McAllen, USA) was guided to the entrance of the ICA and fixed by ligation to the artery and flushed with heparinized saline (2500 IU/ml). The arterial catheter was then connected to an infusion pump (Alaris GH Plus Syringe Pump, CareFusion, Lyngby, Denmark). Through this pump, the pigs received 10 ml/kg BW/h maintenance isotonic saline (Ringer-acetate; Fresenius Kabi AB, Uppsala, Sweden). The pump was also used for infusion of bacteria. The pigs were randomly assigned to the two infusion methods: Pig 1 received bacteria suspended in isotonic saline. The bacterial suspension was infused at maintenance flow rate for exactly 60 min (i.e. 10 ml suspension/kg BW/h). Pigs 2 and 3 received microthrombi suspension at maintenance flow rate for 10 min (Table 1). After infusion, all pigs received sterile saline at maintenance flow rate through a new syringe for 30 min to flush the infusion catheter. After flushing, the ICA was ligated in front of the catheter. The ICA catheter was withdrawn and the surgical incision was prepared with 1 ml bupivacaine (Bupivacain 5 mg/ml, SAD, Amgros I/S, Copenhagen, Denmark) and sutured. Pigs were treated with an IM injection of 0.3 mg buprenorphine (Temgesic, Reckitt Benckiser, Berkshire, UK) before anesthesia was ceased.
Post-operative procedures
The pigs were clinically examined every 4 h from the time of infusion
and treated with 0.3 mg buprenorphine IM every 8 h until euthanasia.
Clinical examinations included evaluation of appearance and general
condition, appetite (feed consumed between clinical examinations),
urination and defecation in the pen, skin elasticity, mucous membrane
color and capillary refill time, heart rate, rectal temperature and
general responsiveness. Responsiveness was measured by ear and eye
movement towards sounds and by the general reaction to human contact.
At each clinical examination the pigs were offered 5 ml of apple juice
through a syringe. The pigs were considered to reach the humane
endpoints if they displayed one or more of the following behaviors: 1)
Lack of urination and/or defecation in the pen since the last clinical
examination combined with reluctance to accept apple juice; 2) Lack of
feed consumption since the last clinical examination combined with
reluctance to accept apple juice; and 3) Reluctance or incapability to
rise and approach the apple juice. Pigs that did not meet the humane
endpoints were euthanized 24 h (Pigs 1 and 2) and 48 h (Pig 3) after
infusion. They were deeply anesthetized by IM injection of 1 ml/kg of
a solution of 125 mg tiletamine hydrochloride and 125 mg zolazepam
hydrochloride suspended in 5 ml followed by 10 ml propofol applied
through an ear vein catheter and finally exsanguinated.
Blood samples
Blood samples were acquired at 24 h before infusion from a venous
puncture, during surgery through the EJV catheter just before infusion
and, through the EJV catheter at the end of the clinical examinations
at 4, 8, 12, 24 and 48 h after infusion. Each blood sample was
immediately divided into three aliquots. The first aliquot was allowed
to coagulate and was used for analyses of acute-phase proteins. The
second aliquot was stabilized with ethylenediaminetetraacetic acid
(EDTA) and used for bacteriological cultivation. The third aliquot was
stabilized with EDTA and used for hematology.
Analysis of acute-phase proteins
Porcine α 1-acid glycoprotein (PAGP) concentrations
were determined by a competitive catching enzyme-linked immunosorbent
assay (ELISA) (Heegaard et al., 2013). All samples were run
twice at 1/500 or higher dilutions with a detection limit of 50 mg/l.
Haptoglobin concentrations were determined by a sandwich ELISA (Soerensen et al., 2006) with a detection limit of 130 mg/l. Serum amyloid A (SAA)
concentrations were determined by a commercially available sandwich
ELISA (Phase SAA Assay, Tridelta Development Ltd., Kildare, Ireland)
(McDonald et al., 1991). Samples were tested according to the
manufacturer’s instructions but a low dilution of 1:20 was used
to increase signal intensity. The detection limit of the assay was
31.3 mg/l (porcine SAA equivalents). Finally, C-reactive protein
(CRP) concentrations were determined by a sandwich ELISA (Heegaard et al., 1998). Polyclonal rabbit anti-human antibodies with cross-reactivity
towards porcine CRP were employed (Heegaard et al., 2009)
followed by peroxidase-conjugated goat anti-rabbit antibody for
detection (DAKO, Glostrup, Denmark). Pooled pig serum calibrated
against a human CRP calibrator (DAKO A0073) was used as a standard.
The detection limit was 0.35 mg/l (human equivalents). Development of
CRP plates was done with a tetramethylbenzidine peroxide color
substrate (Kem-En-Tec, Taastrup, Denmark). All samples including
standards were run in duplicate. Sample values were calculated from
the curve fitted to the readings of the standard (using Ascent
software v. 2.6, Thermo Scientific).
Bacteriology
All blood samples and homogenized samples (10 g) of liver, lung and
spleen were cultured on blood-agar plates for 24 h at 37 °C using both
undiluted and tenfold dilutions (final detection limit: 1 CFU/ml blood
and 1 CFU/g tissue). From each sample with a positive culture, the
colony morphology was evaluated and one colony was selected for
S. aureus protein A typing (spa-typing) with the
inoculated S. aureus strain as the control.A multiplex
polymerase chain reaction technique (Stegger et al., 2012)
and BioNumerics v 6.6 (Applied Maths, Sint-Martens-Latem, Belgium)
were used to amplify, sequence and analyze the spa gene and
assign the spa type.
Hematology
An automated complete blood cell count including neutrophil count was
conducted (ADVIA 120 analyzer, Bayer Healthcare Diagnostics, Berlin,
Germany), as described by Leifsson et al. (2010).
Necropsy, histology and immunohistochemistry
Full necropsies were conducted. Specimens of liver and lung and the
entire brain were fixed by immersion in 10% neutral buffered formalin
and processed by routine methods and paraffin embedded. The brain was
sliced into coronal slabs of 4 mm before paraffin embedding. Sections
of 4 μm were made from each brain slab and
stained with hematoxylin and eosin. Furthermore, IHC staining was
performed for in situ detection of S. aureus antigen
(Kvist et al. 2002), glial fibrillary acidic protein (GFAP)
(Sikasunge et al., 2009), myeloperoxidase for detection of
neutrophils (Christiansen et al., 2013a), and for ionized
calcium binding adapter molecule 1 (IBA-1) to detect microglial cells
and monocytes (Grossi et al., 2015).
Results
Throughout the study, pigs showed only mild clinical signs although they preferred to lie down during the first hours after surgery. Their rectal temperature increased to a maximum of 40.5 °C (acclimatizing temperature 48 h before infusion: 38.1 – 39.5 °C).
Serum levels of acute phase proteins showed that both SAA and
haptoglobin increased with a steep rise in concentration within the
first 24 h after infusion. The level of CRP also increased after
infusion. The level of PAGP was only raised in Pig 2 at 24 h and
remained normal or decreased in the other two pigs (Fig 1). Two blood
samples from Pig 3 yielded too little serum to enable analysis of all
four acute-phase proteins. The missing analyzes for Pig 3 were: all
acute phase proteins at 8 h after infusion and CRP and PAGP at 48 h
after infusion.
No bacteria were cultured from blood or tissues from Pig 3, whereas
S. aureus (same spa-type as infused strain) were isolated
from spleen and lung, and in the blood until 12 h after infusion, in
Pig 2, and in the spleen, lung and liver of Pig 1 (Table 1).
Table 1. Design and results from infusion of Staphylococcus aureus to the brain through the internal carotid artery. All pigs received 108 CFU/kg body weight. Liver, lung, spleen and blood were examined bacteriologically. Blood samples were taken at -48, 0, 4, 8, 12, 24 and 48 h after infusion. Detection limit of bacterial cultures: 1 CFU/ml blood and 1 CFU/g tissue.
|
Pig |
Type of infusion |
Duration of infusion |
Survival time |
Brain lesions |
Bacteriology |
1 |
Bacteria suspended in saline |
60 min |
24 h |
Mild edema |
Spleen (1 CFU/g), lung (9 CFU/g) and liver (5 CFU/g) |
2 |
Bacteria embedded in microthrombi |
10 min |
24 h |
Mild edema |
Blood until 12 h after infusion, spleen (3 CFU/g), lung (1CFU/g) |
3 |
Bacteria embedded in microthrombi |
10 min |
48 h |
Microabscess |
All samples were negative |
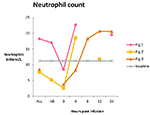
Hematology showed that all pigs developed neutrophilia within 8 h (Fig
2). Some blood samples yielded too little blood to enable analysis.
The missing analyzes were: Pig 1 at 8 and 12 h post infusion; Pig 2 at
8 h post infusion; Pig 3 at 48 h before infusion and 48 h after
infusion.
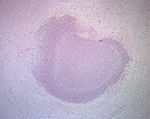
Histology showed that the only brain lesion present in pigs euthanized
at 24 h (Pigs 1 and 2) was slight edema. Pig 3 that was euthanized
after 48 h had a single gray matter microabscess located peripheral to
the right lateral ventricle near the hippocampus (Fig 3). The abscess
consisted of densely organized round cells of which most stained
positive for myeloperoxidase. The myeloperoxidase-negative cells
stained positive for IBA-1. The microabscess comprised mainly of
neutrophils with a rounded morphology but also of monocytes. GFAP IHC
indicated peripheral hypertrophy and proliferation of astrocytes. Due
to the limited size of the abscess only the periphery of the abscess
was included in the slide used for S. aureus antigen
detection. The periphery of the abscess did not stain positive for
S. aureus. As the abscess had already been entirely cut into
the existing slides it was not possible to increase the number of
slides used for S. aureus antigen detection. No lesions were
found in the lung and liver in any of the pigs.
Discussion
We here report the results for local infusion of bacteria to the
porcine brain as a model of sepsis-related brain microabscesses. Our
results show that bacteria suspended in saline or embedded in
microthrombi can pass through the rete mirabile in
pigs. Passage through the rete mirabile was confirmed by
isolating bacteria from the systemic circulation following both
infusion methods. Accordingly, both infusion methods resulted in local
brain bacteremia and systemic bacteremia.
Furthermore, brain bacteremia created by infusion of
S. aureus embedded in microthrombi resulted in microabscess
formation and thereby resembled human cases of
S. aureus sepsis (Pendlebury et al., 1989; Sharshar et al., 2004). The abscess morphology was characterized by rounded neutrophils.
The presence of rounded neutrophils is a rare finding but has
previously been reported in combined experimental porcine
S. aureus sepsis and endocarditis (Astrup et al. 2013;
Christiansen et al., 2013a). Despite the limited number of
pigs in our study, the finding of this particular brain abscess
morphology therefore seems unlikely to be a coincidence. In addition,
former studies have shown that only the center of a microabscess
stains positive for S. aureus (Christiansen et al., 2013a). This seems a likely scenario in our study as well because we could
not detect the bacteria outside the center of the abscess. Our results
indicate that a survival time above 24 h is needed for the development
of significant brain pathology when bacteria are infused locally to
the brain. This is in contrast to sepsis models that apply systemic
bacterial infusion which results in brain microabscesses developing
earlier and in higher numbers (Astrup et al., 2013).
Concerning the clinical course, our results indicate that models of
local brain infusion of bacteria are much more beneficial in terms of
decreased animal suffering and management challenges compared with
ordinary sepsis models (Nemzek et al. 2008;
Leifsson et al., 2010; Soerensen et al., 2012; Christiansen et al.,
2013b).
Collectively, fever, neutrophilia, activated acute-phase response and
bacteremia show that all pigs developed sepsis as defined by the
criteria for the systemic inflammatory response syndrome (Levy et al., 2003). However, former models that have applied the same bacterial strain
and dose systemically have resulted in severe sepsis with a mortality
rate of 60% within 48 h of infection (Soerensen et al., 2013). Contrary to this, our pigs did not develop severe sepsis and the
mortality rate was 0. It may therefore be speculated that the
sepsis-reaction per se affects the development of brain
microabscesses. Such sepsis influence on the brain may include
cytokine-induced permeability of the blood-brain-barrier and anoxic
damage to neurons (Sharshar et al., 2003, Sharshar et al., 2005). As such, sepsis-effects on the brain might ease the spread of
bacteria from the blood to the brain parenchyma and thus affect the
number and development time of brain microabscesses. Therefore, the
sparse clinical effects with our infusion models may hypothetically
also account for the decreased brain pathology despite the direct
brain infusion design.
In conclusion, this study shows that brain bacteremia in pigs can be
created by using either of our local infusion methods despite the
presence of a rete mirabile in pigs. Also both infusion
methods apparently avoid the development of severe clinical signs as
observed in sepsis-models that apply systemic bacterial infusion.
Furthermore, local brain infusion with S. aureus embedded in
autologous microthrombi resulted in sepsis-related brain pathology
with a microabscess as the most characteristic lesion. We therefore
recommend the microthrombi-infusion method to be further developed as
it has the potential to meet the strong demand for both reduction and
refinement of existing sepsis models.
Competing interests
The authors declare that they have no competing interests.
Acknowledgments
The authors would like to thank Andreas Vegge for his contributing
advice in the surgical design. The work was financed by grant no.
271-07-0417 from the Danish Medical Research Council, and by Aase og
Ejnar Danielsens Fond.
References
- Astrup LB, MV Nielsen, TM Iburg, PS Leifsson, HE Jensen, OL Nielsen & JS Agerholm: Brain microabscesses in a porcine model of Staphylococcus aureus sepsis. Acta Vet. Scand. 2013, 55, 76.
-
Azuma A, K Toyoda & T O’uchi: Brain magnetic
resonance findings in infective endocarditis with neurological
complications. Jpn. J. Radiol. 2009, 27, 123-130.
-
Bogdanski R, M Blobner, I Becker, F Hänel, H Fink & E Kochs: Cerebral histopathology following portal venous infusion of
bacteria in a chronic porcine model. Anesthesiology. 2000,
93, 793-804.
-
Christiansen JG, M Oscarson, HE Jensen, LK Jensen, J Koch, B
Aalbæk, OL Nielsen, TM Iburg & PS Leifsson: Embolic encephalitis in a porcine model of endocarditis. In Vivo.
2013a, 27, 591-597.
-
Christiansen JG, HE Jensen, LK Johansen, J Koch, J Koch, B
Aalbaek, OL Nielsen & PS Leifsson: Porcine models of non-bacterial thrombotic endocarditis (NBTE) and
infective endocarditis (IE) caused by Staphylococcus aureus: A
preliminary study. J. Heart. Valve. Dis. 2013b,
22, 368-376.
-
Grossi AB, P Hyttel, HE Jensen & PS Leifsson: Porcine
melanotic cutaneous lesions and lymph nodes: immunohistochemical
differentiation of melanocytes and melanophages. Vet. Pathol.
2015, 52, 83-91.
-
Haaland K & WJ Orderud: The piglet as a model for
cerebral circulation: an angiographic study. Biol. Neonate. 1995,
68, 75-80.
-
Hasman H, A Moodley, L Guardabassi, M Ategger, RL Skov & FM
Aarestrup: Spa type distribution in Staphylococcus aureus originating
from pigs, cattle and poultry. Vet. Microbiol. 2010, 141, 326–331.
-
Heegaard PMH, J Klausen, JP Nielsen, N Gonzáles-Ramón, M Piñeiro,
F Lampreave & MA Alava: The porcine acute phase response to infection with
Actinobacillus pleuropneumoniae. Haptoglobin, C-reactive
protein, major acute phase protein and serum amyloid A protein are
sensitive indicators of inflammation. Comp. Biochem. Physiol. 1998,
119B, 365-373.
-
Heegaard PMH, HG Pedersen, AL Jensen & U Boas: A robust
quantitative solid phase immunoassay for the acute phase protein
C-reactive protein (CRP) based on cytidine 5’-diphosphocholine
coupled dendrimers. J. Immunol. Meth. 2009, 343, 112-118.
-
Heegaard PMH, I Miller, NS Sorensen, KE Soerensen & K
Skovgaard: Pig α 1-acid glycoprotein: Characterization and
first description in any species as a negative acute phase protein.
PLOS ONE. 2013, doi:10.1371.
-
Kvist PH, ES Jensen, B Aalbæk & HE Jensen: Evaluation
of the pathology, pathogenesis and aetiology of auricular
elephantiasis in slaughter pigs. J. Vet. Med. 2002, 49,
517-522.
-
Leifsson PS, TM Iburg, HE Jensen, JS Agerholm, M
Kjeldgaard-Hansen, B Wiinberg, PMH Heegaard, LB Astrup, AE Olsson,
MG Skov, B Aalbaek & OL Nielsen: Intravenous inoculation of Staphylococcus aureus in pigs
induces severe sepsis as indicated by increased hypercoagulability
and hepatic dysfunction. FEMS. 2010, 309, 208-216.
-
Levy MM, MP Fink, JC Marshall, E Abraham, D Angus, D Cook, J
Cohen, SM Opal, JL Vincent & G Ramsay: 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions
conference. Crit. Care Med. 2003, 31, 1250-1256.
-
McDonald TL, A Weber & JW Smith: A monoclonal antibody
sandwich immunoassay for serum amyloid A (SAA) protein. J. Immunol.
Meth. 1991, 144, 149-155.
-
Nemzek JA, KMS Hugunin & MR Opp: Modeling Sepsis in the
Laboratory: Merging Sound Science with Animal Well-Being. Comp. Med.
2008, 58, 120-128.
-
Nielsen OL, T Iburg, B Aalbaek, PS Leifsson, JS Agerholm, P
Heegaard, M Boye, S Simon, KB Jensen, S Christensen, K Melsen, AK Bak, ER Backman, MH Jørgensen, DK Groegler, AL Jensen,
M Kjelgaard-Hansen & HE Jensen: A pig model of acute Staphylococcus aureus induced pyemia.
Acta Vet. Scand. 2009, 51, 14.
-
Pendlebury WW, DP Perl & DG Munoz: Multiple
microabscesses in the central nervous system: a clinicopathologic
study. J. Neuropathol. Exp. Neurol. 1989, 48, 290-300.
-
Reinert M, C Brekenfeld, P Taussky, R Andres & RW Seiler: Cerebral revascularization model in a swine. Acta Neurochir.
2005, Suppl 94, 153-157.
-
Sharshar T, F Gray, G Lorin de la Grandmaison, NS Hopkinson, E
Ross, A Dorandeu, D Orlikowski, JC Raphael, P Gajdos & D
Annane: Apoptosis of neurons in cardiovascular autonomic centres triggered
by inducible nitric oxide synthase after death from septic shock.
Lancet. 2003, 362, 1799-1805.
-
Sharshar T, D Annane, G Lorin de la Grandmaison, JP Brouland, NS
Hopkinson & F Gray: The neuropathology of septic shock. Brain Pathol. 2004,
14, 21-33.
-
Sharshar T, NS Hopkinson, D Orlikowski & D Annane: Science
review: The brain in sepsis – culprit and victim. Crit. Care. 2005,
9, 37-44.
-
Sikasunge CS, MV Johansen, IK Phiri, AL Willingham & PS
Leifsson: The immune response in Taenia solium neurocysticercosis in
pigs is associated with astrogliosis, axonal degeneration and
altered blood–brain barrier permeability. Vet. Parasitol. 2009,
160, 242-250.
-
Sorensen NS, C Tegtmeier, LO Andresen, M Piñeiro, MJ Toussaint,
FM Campbell, F Lampreave & PMH Heegaard: The porcine acute phase protein response to acute clinical and
subclinical experimental infection with
Streptococcus suis Vet. Immunol. Immunopathol. 2006,
113, 157-168.
-
Soerensen KE, OL Nielsen, MM Birck, DB Soerensen, PS Leifsson, HE
Jensen, B Aalbaek, AT Kristensen, B Wiinberg, M Kjelgaard-Hansen,
PMH Heegaard & TM Iburg: The use of sequential organ failure assessment parameters in an
awake porcine model of severe Staphylococcus aureus sepsis.
APMIS. 2012, 120, 909-921.
-
Stegger M, PS Andersen, A Kearns, B Pichon, MA Holmes, G Edwards,
F Laurent, C Teale, R Skov & AR Larsen: Rapid detection, differentiation and typing of
methicillin-resistant Staphylococcus aureus harbouring
either mecA or the new mecA homologue mecA(LGA251). Clin. Microbiol.
Infect. 2012, 18, 395-400.
- Tunkel AR & D Kaye: Neurologic complications of infective endocarditis. Neurol. Clin. 1993, 11, 419-440.