Original scientific article
Severe bradycardia and hypotension in anaesthetized pigs: Possible interaction between octreotide, xylazine, and atropine: A case series
by Marte Kierulf Åm1, Ingrid Anna Teigen1,
Sven Magnus Carlsen1,2, Sverre Christian Christiansen1,2
1Department of Clinical and Molecular Medicine, Faculty of Medicine
and Health Sciences, Norwegian University of Science and Technology
(NTNU), Trondheim, Norway
2Department of Endocrinology, St Olav’s Hospital, Trondheim,
Norway
Correspondence: Marte Kierulf Åm, mail: marte.k.am@ntnu.no, NTNU, Fakultet for medisin og helsevitenskap, Institutt for klinisk og molekylær medisin (IKOM), P.O.Box 8905, 7491 Trondheim, Norway
Summary
Pigs are common animal models in diabetes research. Streptozotocin-induced destruction of pancreatic β-cells is used to induce diabetes in conscious pigs. However, in short-term non-recovery experiments, suppression of endogenous insulin secretion can be faster and more easily achieved with somatostatin analogues. We report a series of severe and unexpected episodes of severe bradycardia in eight pigs during non-recovery experiments with the original aim of investigating the pharmacokinetics and pharmacodynamics of intraperitoneal hormone delivery. The adverse events occurred four to five hours into the experiments, and we believe that they were caused by an interaction between the somatostatin analogue octreotide, and the sedative drug xylazine and that atropine delayed the time of occurrence.
Introduction
Our research group conducted 44 non-recovery experiments of 8-9 hours duration on healthy pigs between January 2017 and July 2020, to study the pharmacokinetics and pharmacodynamics of intraperitoneal (IP) delivered insulin and glucagon. These experiments were used to develop control algorithms for an artificial pancreas eventually to be used by patients with diabetes. In the spring of 2019, the production of Stresnil ® (azaperone), which we used for premedication, was discontinued. As no equivalent drug was available at the time, we had to change our premedication protocol. After this change, we observed severe bradycardia and hypotension in eight of the experiments and in this paper we discuss the probable cause.
The experiments were approved by the Norwegian Food Safety Authority
(FOTS number 12948) and were in accordance with «The Norwegian
Regulation on Animal Experimentation» and «Directive 2010/63/EU on the
protection of animals used for scientific purposes
».
Materials & Methods
All 44 farm pigs (Sus scrofa domesticus) with a mean weight of 41.6 (SD 7.1) kg (males, n=12) were purchased from the University’s regular supplier and brought to the animal facility a week before the experiments and acclimatised to the new environment and staff. They were held in groups of two to three whenever possible. The pens were 5.6 m2 and had solid concrete floors, including an elevated area with a half cover and heating lamp. Wood chips (Lantbruksströ,Yesbox, Skutskär, Sweden) were provided as bedding and nesting material. The pigs were offered toys to keep them occupied, such as balls made of hard plastic, and cardboard boxes. They were fed twice a day with a standard commercial growth feed (Format Vekst 110, Felleskjøpet, Lillestrøm, Norway) and provided with tap water from drinking nipples ad libitum. The lighting conditions were standardised with a 12-hour light period with a gradual transition (05:00 - 07:00 and 19:00 - 21:00) to an eight-hour period without light. The room temperature was 21-22 °C, humidity 29-35% and the ventilation rate was set at 15-20 air changes per hour.
Because azaperone was not available from the spring of 2019, we
changed our premedication protocol from an intramuscular injection of
0.15 mg/kg diazepam (Stesolid ®, Actavis Group , Hafnarfjordur, Iceland), 5.5 mg/kg azaperone (Stresnil
®, Eli Lilly Regional Operations GmbH, Austria) and 25 mg/kg
ketamine (Ketalar ®, Pfizer AS, Norway ) (Åm et al. 2020) to a
combination of 2 mg/kg xylazine (Xysol ®, CP-Pharma Handelsges mbH, Germany) and 20 mg/kg ketamine (Ketalar
®, Pfizer AS, Norway ). Sixteen experiments were conducted using the latter premedication,
eight of the 16 pigs were females, the mean body weight was 42.4 kg
(SD 5.56), and they were around 3-4 months old (Figure 1). No other
changes were made to the protocol, and anaesthesia was induced by
intravenous (IV) injections of 150-250 µg fentanyl (Actavis Group,
Hafnarfjordur, Iceland), 75-125 mg thiopental (VUAB Pharma AS,
Roztoky, Czech Republic) and 150-250 mg ketamine. Atropine, 1 mg,
(Takeda AS, Asker, Norway) was given IV immediately before the
induction of anaesthesia. The trachea was intubated, and lungs
mechanically ventilated to maintain normocapnia (Aisys, GE Healthcare
Technologies, Oslo). Ventilation was volume-controlled with 10 ml/kg
as a general setting but with individual adjustments and a positive
end-expiratory pressure of around 4-5 cm H2O. Anaesthesia was
maintained by IV infusion of midazolam (0.5 mg/kg/h) (Accord
Healthcare Limited, Middlesex, UK) and fentanyl (7.5 µg/kg/h), and by
inhalation of isoflurane (0.5-2.0% adjusted according to anaesthesia
depth) (Baxter AS, Oslo, Norway). Fluid balance was achieved by
continuous IV infusion of Ringer’s acetate, approximately 125
ml/h with individual adjustments. Blood pressure was measured with an
intraarterial pressure sensor in the left carotid artery, oxygen
saturation was measured with a pulse oximeter clamped on an ear and
core temperature was continuously monitored by a rectal thermometer.
All vital signs were continuously monitored on an anaesthesia machine
(Aisys, GE Healthcare Technologies, Oslo). Metabolites and
electrolytes were analysed with ABL 800 Flex blood gas analyzer
(Radiometer Medical ApS, Brønshøj, Denmark).
Catheters were inserted in the left carotid artery and left internal
jugular vein, through the same cut-down. A bladder catheter was placed
by exposing the bladder through a small, low laparotomy, and one or
two catheters from insulin pumps were placed in the upper parts of the
intraperitoneal space through an incision 2-3 cm caudally to the
umbilicus. Cephalothine (Cefalotin, Villerton Invest SA, Luxembourg) 2
g, was given IV every fourth hour. Endogenous secretion of insulin and
glucagon was suppressed by IV boluses of 0.4 mg octreotide
(Sandostatin 200 µg/ml, Novartis Europharm Limited, United Kingdom)
every hour and subcutaneous injections of 0.3 mg pasireotide
(Signifor 0.3 mg/ml, Novartis Europharm Limited, United Kingdom)
every third hour. The first bolus dose of a somatostatin analogue was
given approximately 90 minutes after the premedication. Further
descriptions of experiments with similar set up can be found in our
previous publications (Åm et al. 2020; Dirnena-Fusini et al. 2021).
The animals were euthanised at the end of the eight to nine-hour
experiments by an IV overdose of pentobarbital (minimum 100 mg/kg)
(pentobarbital NAF, Apotek, Lørenskog, Norway).
Results
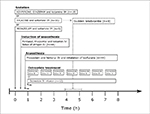
Severe bradycardia and hypotension were observed in eight of 16 experiments (male, n=5), between May 2019 and December 2019 when xylazine and ketamine was used as premedication (Figure 1). The adverse effects occurred four to five hours after the pigs were premedicated. The heart rate dropped from 100 (SD 16.1) beats per minutes (bpm) to 59 (SD 17.5) bpm, within one second. The blood pressure fell simultaneously from 93 (SD 4.4)/61 (SD 5.0) mmHg with a mean arterial pressure (MAP) of 75 (SD 3.7) mmHg to 73 (SD 4.8) /39 (SD 7.3) mmHg with a MAP of 52 (SD 6.6) mmHg. Blood glucose was measured at least every 20 minutes, and more often when deemed necessary to avoid hyper-or hypoglycemia. The pigs were normothermic, euglycemic and showed normal electrolyte and lactate values throughout the experiments. There were no triggering actions or visible warnings before the occurrence of the adverse effects. At the onset of the cardiovascular adverse effects, six of eight affected pigs showed temporary muscle spasms lasting a few seconds, especially in the front legs. The IV fluid infusion was increased after the occurrence of adverse effects, but no other interventions were made. Two of the affected pigs were euthanized at six and 30 minutes after the onset of the cardiovascular adverse effects. The other six pigs showed a slow but steady improvement in both heart rate and blood pressure over one to two hours. No pigs showed signs of regaining consciousness and we regarded the welfare of the animals as uncompromised. As this paper is a description of a case series, there are no control groups. However, no similar cardiovascular adverse effects were observed in 21 one-day non-recovery experiments for testing of surgical equipment under development and training of surgical teams conducted by other research groups at NTNU’s Comparative Medicine Core Facility (CoMed) using the same protocol for premedication and anaesthesia, but without the use of octreotide, after May 2019 (personal communication Oddveig Lyng), or in the 19 experiments we conducted before May 2019 (Dirnena-Fusini et al. 2021; Åm et al. 2020) (Figure 1).
|
Figure 1: Schematic presentation of the anaesthetic protocol
with number of animals and changes in sedation and octreotide
treatment indicated. Click image to enlarge |
We made several adjustments to the study protocol, in separate
experiments, to determine and eliminate the cause of these adverse
cardiovascular effects. This included increasing fluid replacement,
reducing the dose of somatostatin analogues, omitting pasireotide and
giving octreotide as an infusion rather than hourly boluses. However
these adjustments did not eliminate the adverse effects. Finally, we
replaced xylazine with 0.8 mg/kg midazolam in the premedication
mixture with ketamine. No episodes of severe bradycardia were observed
in the nine consecutive pig experiments conducted in the spring of
2020 when xylazine was omitted from the premedication mixture (Figure
1) (males, n=4).
Discussion
Several of the drugs included in our original and adjusted premedication and anaesthesia protocol can cause cardiovascular adverse effects, such as ketamine, midazolam, fentanyl, thiopental and xylazine. Also octreotide is reported to cause bradycardia (Herrington et al. 1998; Icen et al. 2019). Until May 2019, we used a well-established protocol for premedication and anaesthesia, in which the pigs were sedated with an IM injection of diazepam, azaperone and ketamine without observing any serious cardiovascular adverse effects. The cardiac adverse effects were only observed when xylazine was given as a part of the premedication, making xylazine the most likely candidate to have caused the observed phenomenon. Xylazine is a sedative drug commonly used for cattle, sheep, dogs, cats and horses in clinical treatment. It is not widely used in pigs, but for research purposes it is sometimes used as a premedication to anaesthesia in combination with other drugs. Xylazine is an alpha-2 agonist and as all of the drugs in this group it can cause a variety of adverse effects , including bradycardia, respiratory depression, hypotension and reversible arrhythmias (CP-Pharma, 2012). The negative impact on the cardiovascular system caused by alpha-2 agonists is actually a result of two different effects, namely a diminished sympathetic tone and increased systematic vascular resistance (Sinclair 2003). These adverse effects typically occur shortly after drug delivery. However, we observed the adverse cardiac effects four to five hours after administrating xylazine. Because similar adverse effects were not observed in experiments conducted by other research groups at our university also using xylazine as a premedication drug, it is unlikely that xylazine was the sole cause of the observed cardiovascular adverse effects.
The use of somatostatin analogues is one of the major differences
between our experiments and the other non-recovery experiments
conducted at CoMed. Somatostatin analogues mimic the effects of the
natural hormone somatostatin and inhibit the release of several
hormones. The drugs are used in human clinical practice to suppress
the secretion of growth hormone in patients with acromegaly, and to
suppress excessive hormone release from certain pancreatic and
gastro-enteral neuroendocrine tumours (Lamberts and Hofland 2019). In
diabetes research, the drugs are used to inhibit the secretion of
insulin and glucagon in animal models.
In addition to the suppressive effects on hormone secretion,
octreotide affects a wide variety of metabolic pathways including the
inhibition of enzymes in the cytochrome P450 family (CYP) in humans
(Rasmussen et al. 1998; Rendic 2002). The majority of these enzymes
are expressed in the liver (Zanger and Schwab 2013), where they form a
complex system which is responsible for metabolizing around 70-90% of
the drugs in clinical use (Zanger and Schwab 2013; Preissner et al.
2013). Inhibition of CYP will lead to delayed metabolism and potential
accumulation of several of the drugs used in our experiments,
including xylazine (Veilleux-Lemieux et al. 2013) and atropine (Van
der Meer et al. 1983).
We speculate that the late onset of bradycardia is explained by the
routine administration of atropine at the time of inducing
anaesthesia. Atropine is a competitive muscarinic acetylcholine
receptor antagonist and has a vagolytic effect on the sinus node
(Schweitzer & Mark 1980), counteracting bradycardia. In fact,
atropine is used in clinical practise as a treatment and way of
preventing bradycardia caused by xylazine and other alpha-2 agonists.
However, the overall benefit of giving atropine to counteract or
prevent alpha-2 agonist mediated bradycardia and decreased cardiac
output is debated, and conflicting arguments are expressed (Sinclair
2003). Atropine has a reported half-life of around 40 minutes in pigs
weighing 58-71 kg (Loughren 2016). The diminishing concentration of
atropine hours after administration, and the potentially prolonged
high levels of xylazine, may explain how xylazine could cause severe
bradycardia four to five hours after administration.
To conclude, even with the limitations of a case series, we believe that the sudden and severe bradycardia and hypotension observed in our set of non-recovery experiments on pigs were caused by an interaction between octreotide and xylazine, and that atropine delayed the time of onset. This information could be of high relevance to other researchers working with pigs as an animal model in diabetes research.
Data availability
Additional data are available upon request.
Conflict of interests
All authors declare no conflict of interests.
Author contributions
MKÅ completed the trial, collected and analysed the data, wrote and edited the manuscript, and is the guarantor of the work. SMC and SCC contributed to the development of the protocol and the discussion, reviewed and edited the manuscript. IAT reviewed and edited the manuscript.
Acknowledgments
The animal experiments were performed at the Comparative Medicine Core Facility (CoMed) at Norwegian University of Science and Technology (NTNU).
The Double Intraperitoneal Artificial Pancreas project is part of the
Centre for Digital Life Norway and supported by the Research Council
of Norway (grant number 248872). The work was also supported by a
scholarship from the Central Norway Regional Health Authority (grant
number 2014/23166) and the Norwegian Medical Association Johan Selmer
Kvanes Endowment. The funding sources had no role in the collection,
analysis, interpretation or publication of the data.
References
- CP-Pharma, (2012). Xylazine 100 mg/ml, solution for injection. Packaging, Labelling and Package Leaflet. Available at: https://mri.cts-mrp.eu/Human/Downloads/NL_V_0158_002_FinalPI.pdf (Accessed: 5.11.2021).
- Dirnena-Fusini, I., Åm, M.K . , Fougner, A.L., Carlsen, S.M., Christiansen, S.C., (2021). Intraperitoneal insulin administration in pigs: effect on circulating insulin and glucose levels. BMJ Open Diabetes Research and Care. 9, e001929. https://doi.org/10.1136/bmjdrc-2020-001929
- Herrington, A.M., George, K.W., Moulds, C.C., (1998). Octreotide-induced bradycardia. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy. 18(2), 413–416. https://doi.org/10.1002/j.1875-9114.1998.tb03872.x
- Icen, Y.K., Urgun, O.D., Sumbul, H.E., Koc, M., (2019). Complete heart block due to octreotide infusion in patient with cryptogenic cirrhosis. The Eurasian Journal of Medicine. 51(1), 95–97. https://doi.org/10.5152/eurasianjmed.2018.18064'
- Lamberts, S.W., Hofland, L., (2019). Anniversary review: Octreotide, 40 years later. European Journal of Endocrinology. 181(5), 173–183. https://doi.org/10.1530/EJE-19-0074
- Loughren, M.J., (2016). Pharmacokinetics of IM, IV and IO atropine in normovolemic and hypovolemic swine. Available at: https://apps.dtic.mil/sti/pdfs/AD1028154.pdf (Accessed: 10.11.2021).
- van der Meer, M.J., Hundt, H.K., Müller, F.O ., (1983). Inhibition of atropine metabolism by organophosphate pesticides. Human Toxicology. 2(4), 637–640. https://doi.org/10.1177/096032718300200409
- Preissner, S.C., Hoffmann, M.F., Preissner, R., Dunkel, M., Gewiess, A., Preissner, S., (2013). Polymorphic cytochrome P450 enzymes (CYPs) and their role in personalized therapy. PloS one. 8(12), p.e82562. https://doi.org/10.1371/journal.pone.0082562
- Rasmussen, E., Eriksson, B., Oberg, K., Bondesson, U., Rane, A., (1998). Selective effects of somatostatin analogs on human drug-metabolizing enzymes. Clinical Pharmacology and Therapeutics. 64(2), 150–159. https://doi.org/10.1016/S0009-9236(98)90148-5
- Rendic, S., (2002). Summary of information on human CYP enzymes. Drug Metabolism Reviews. 34(1-2), 83–448. https://doi.org/10.1081/DMR-120001392
- Schweitzer, P., Mark, H., (1980). The effect of atropine on cardiac arrhythmias and conduction. Part 1. American Heart Journal. 100(1), 119–127.
- Sinclair, M.D., (2003). A review of the physiological effects of alpha2-agonists related to the clinical use of medetomidine in small animal practice. The Canadian Veterinary Journal. La Revue Vétérinaire Canadienne. 44(11), 885–897.
- Veilleux-Lemieux, D., Castel, A., Carrier, D., Beaudry, F., Vachon P., (2013). Pharmacokinetics of ketamine and xylazine in young and old Sprague-Dawley rats. Journal of the American Association for Laboratory Animal Science. 52(5), 567–570.
- Zanger, U.M., Schwab, M., (2013). Cytochrome P450 enzymes in drug metabolism: regulation of gene expression, enzyme activities, and impact of genetic variation. Pharmacology & therapeutics. 138(1), 103–141. https://doi.org/10.1016/j.pharmthera.2012.12.007
- Åm, M.K. , Dirnena-Fusini, I., Fougner, A.L., Carlsen, S.M., Christiansen, S.C., (2020). Intraperitoneal and subcutaneous glucagon delivery in anaesthetized pigs: effects on circulating glucagon and glucose levels. Scientific Reports. 10(1), 1–8. https://doi.org/10.1038/s41598-020-70813-5